Osteoporosis
At LSARA, we offer expedited Bone Clinic appointments to quickly review and address Osteoporosis.
Osteoporosis Topic Guide
Bone Health Clinics for Osteoporosis
Your first 3-4 visits will be with an osteoporosis specialist so that they may evaluate your current disease state and begin treatment. Once you are ready for maintenance care, you will be transferred to a care team within our regular rheumatology treatment for long-term care and monitoring.
Your visits to the Bone Clinic may include:
- DEXA and lab review
- Patient education regarding dietary changes
- Initiation of medication therapies
We offer Bone Clinic appointments within 1-2 weeks – contact us to schedule by calling 817-789-6770!
Please be ready to provide your most recent DEXA scan and any relevant chart notes.
What is Osteoporosis?
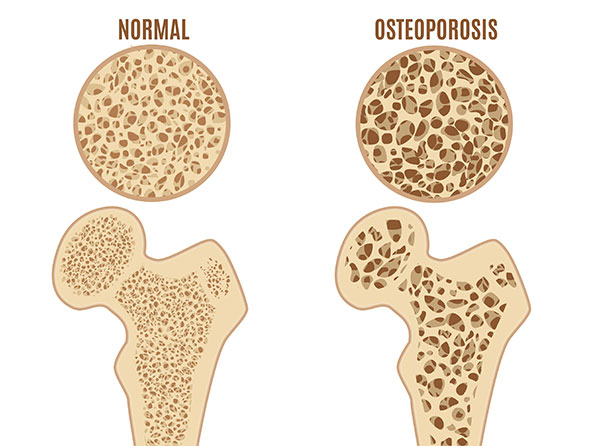
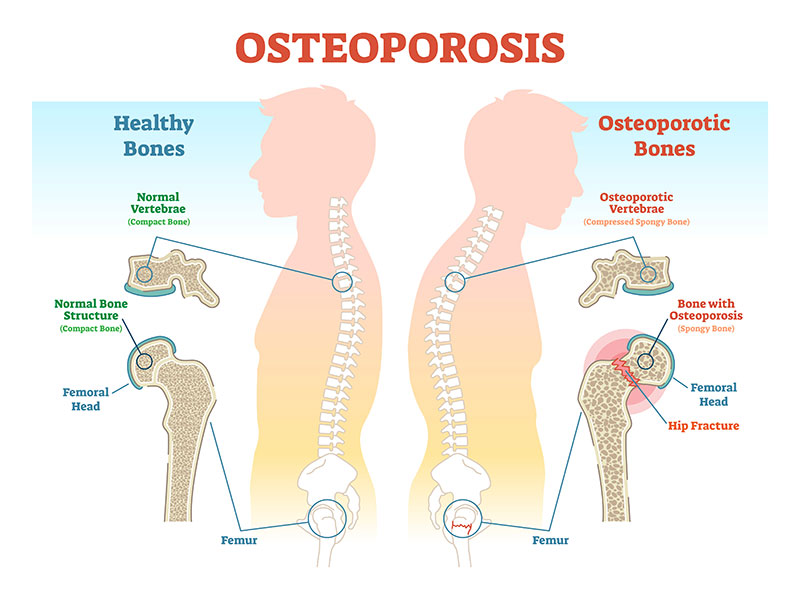
Osteoporosis (OP) is a degenerative bone disease that causes bone loss which makes bones weak of the skeleton and brittle to the point that even mild stress or a minor fall can cause fractures. The most common fracture sites in OP patients are the hip, wrist, or spine. But upper arm, rib, and pelvic fractures are often due to osteoporosis outside of significant trauma.
Bone is living tissue regularly broken down and replaced in remodeling; osteoporosis happens when the creation of new bone cannot keep up with the bone loss. There are too many bone withdrawals and not enough bone deposits. Treatment focuses on stopping bone loss, increasing bone growth, and ultimately increasing the strength of all the skeleton bones.
While osteoporosis affects both men and women of all races, white and Asian women, especially post-menopausal, are at the highest risk.

Symptoms of Osteoporosis
There are typically no symptoms when bone loss is in its early stages. Once osteoporosis weakens bones to a significant degree, the following symptoms may occur:
- Back pain which is caused by collapsed or fractured vertebra
- Bones that break more quickly than they should and usually cause pain
- Stooped posture
- Loss of overall height over time
Causes and Risk Factors of Osteoporosis
As we age, bone loss happens faster than bone growth, resulting in osteoporosis. Replacement of old bone with new bone begins to slow down after your 20s; most people reach peak bone mass by age 30. Peak bone mass varies depending on ethnic group, genetic inheritance, and environmental factors.

Risk Factors
- Sex – women are more likely to develop OP than men.
- Age – the older you are, the more likely you are to develop OP.
- Race – people of white or Asian descent.
- Family history – having a parent or sibling with osteoporosis (especially a parent with a hip fracture, no matter what age) puts you at higher risk.
- Body frame size – men and women with smaller frames are at greater risk as their peak bone mass is less.
- Hormones – too much or too little of certain hormones can affect your OP risk level.
Dietary Factors
- Calcium intake – if you lack calcium over your lifetime, it can contribute to diminished bone density, early bone loss, and increased risk of fractures.
- Eating disorders – eating disorders resulting in decreased food intake and causing individuals to be underweight can weaken bones in men and women.
- GI surgery – surgery that removes parts of the intestines or reduces the size of your stomach, reducing the amount of surface area available to absorb nutrients such as calcium.
- Medical diseases such as Rheumatoid Arthritis.
- Certain medications, especially corticosteroids (prednisone).
How is Osteoporosis Diagnosed?
Any adult over 50 (especially post-menopausal females who have lost their estrogen protection for skeletal strength) who suffers a non-traumatic fracture of the skeletal sites mentioned above should be considered and diagnosed as having osteoporosis. Aging weakened skeletons that are fracturing is the fundamental principle defining osteoporosis.
A type of X-Ray bone density scan called a DEXA (DXA) scan can be used to measure and monitor your bone density by determining the proportion of minerals in your bones.
DEXA scans are available at many of our locations to make it easy for you to get a baseline. Then follow-up DEXA scans at appropriate intervals will initially diagnose and carefully monitor for any bone mineral density changes, up or down.
Treatment for Osteoporosis
It is important to understand the goal of treating osteoporosis: strengthening the skeleton to reduce fracture risk. Not always do the DEXA scans show increases in bone mineral density. The medical provider will evaluate each patient to determine the risk of breaking a bone within the next ten years. If the risk level is low, a patient may not yet need medications. The focus may be on modifying behaviors to decrease risk, ensuring proper calcium, vitamin D, and dietary habits, and including anti-gravity exercise (walking is a great example) in one’s lifestyle. Physical therapy interventions to decrease fall risk are advised for patients who fall or are at risk of falling.
Many medications are available for treating osteoporosis. The primary medications are oral, including Fosamax, Boniva, Actonel, and Evista. These are usually the first-line medications relied upon for uncomplicated and less severe OP. They are often demanded to be tried first by various payers as they are less expensive.
For patients who cannot tolerate them and/or for patients with severe disease, often including fractures, a second group of more potent medications exist (which are more expensive):
Lone Star Arthritis & Rheumatology Associates for Osteoporosis Treatment Options
We offer Bone Clinic appointments within 1-2 weeks – contact us to schedule by calling (817) 789-6770! Please be ready to provide your most recent DEXA scan and any relevant chart notes.